Authored by David Wagner (BS Brain & Cognitive Sciences) & Edited by Gaurav Dubey (MS Biotechnology)
High-Quality, Evidence-Based Scientific Content Brought to you by Karmik, LLC
Drug addiction is a pervasive public health issue throughout modern western society, afflicting individuals across all socioeconomic stratifications, races, genders, and ethnic backgrounds. Each year, significant medical and economic resources are deployed to treat drug and alcohol addiction, and yet, despite the politico-medical effort to stalwart the “disease” of addiction, it remains one of the most pressing social issues of our time. Currently, modern science and addiction medicine have failed to produce an effective, universal answer for resolving drug addiction, instead relying on big pharma to reverse engineer a solution to a problem they have largely created, or rehabilitation programs based on 12-step facilitation (TSF) that have questionable clinical efficacy and effectiveness.1, 2
Indeed, the current (and past) focus of drug addiction treatment (and for many, subsequent involvement in the criminal justice system) seems to reinforce a contraction of consciousness and brain activity, continued dependence on mind-altering substances, and a triggering of core trauma through punitive care models. Understanding and applying information about states of consciousness, rooted in transpersonal psychology and modern cognitive science, could provide a platform for a new lens to view addictive behavior and, more importantly, for how to develop effective strategies to transmute those brain states into integrated functioning.

The Development of the Modern Addiction Treatment (Management) Model
Modern addiction treatment has progressed immensely from its dark roots. William White’s 1998 book, Slaying the Dragon: The History of Addiction and Treatment in America, provides an archival presentation of the formation of today’s addiction treatment model. The book follows the placing of alcoholics and addicts on inebriate farms in the early 1900s, the utilization of narcotic drugs for dependency maintenance in the 1920s, psychosurgery, and electroshock therapies in the 1940s, and the formation of specialized TSF rehabilitation centers in the mid-century— the model of treatment that has remained largely unchanged since. Furthermore, the combination of TSF-based addiction treatment and the criminal justice system in the early 90s, with the creation of drug treatment courts and court-mandated substance abuse treatment, provided the combination of law enforcement and the promise of medicine to create a new platform for managing addiction. In the last decade, the re-emergence of the wide-scale use of narcotic and psychotropic medications to manage dependency and treat underlying psychological issues has become the standard of care. The combination of medication therapies and TSF-based rehabilitation is the current gold standard in addiction care and management, and by some accounts contributes to a decreased overdose rate, decreased risk of relapse, and a reduction in infectious diseases like HIV.3
On The Surface, It Would Appear We’ve Optimized a More Efficacious Treatment for Managing Addiction
On face value, it would appear that we have optimized a system for managing addiction as a chronic illness, and compared to previous attempts in history to manage addicts, it seems as though we have moved to a better standard of care for addiction management. The ideal goal of successfully treating and resolving addiction, however, seems to have been lost in the current model of addiction management. In the context of addiction management, we have shifted the entire idea from resolving the roots of addiction and addictive behavior to psychopharmaceutical and behavioral management (generally through negative reward reinforcement at least in current models of treatment). It may well be time to update the management-based approach to addiction to incorporate ideas and practices that could help the addict change the brain state employed by addiction and transform their baseline level of consciousness away from the contracted state of consciousness that addiction itself facilitates and the dissociated state of consciousness that the current management-based system may serve to maintain.
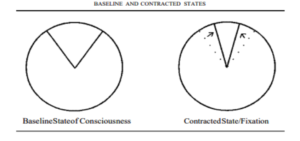
Addiction as a Contracted State of Consciousness: The Spherical Field of Awareness Thought-Model
Ralph Metzer proposed a thought model of consciousness as a “spherical field of awareness that surrounds us and moves with us everywhere we go”.4 For simplification purposes, we will work with one 2-D slice of this sphere of consciousness. This horizontal plane section of the spherical field gives us a 360° circle of “potential awareness,” or a potential focus of attention. We will assume that in our baseline state of consciousness we utilize only 45° of the available 360° consciousness field.

In Active Addiction, Our Attention Becomes Extremely Narrow
In active addiction, our attention becomes extremely narrow; our focus on a singular purpose (getting and using our drug of choice) becomes hyper-vigilant, and our brain activity becomes more organized and synchronous (resulting in a net increase in rigidity or decrease in adaptability). We effectively decrease our field of potential awareness down to 30°, 15°, or even just 1° of the total possible experience of consciousness. The external object of desire, the craved sensation, the bottle, pipe, etc., becomes the slice of potential awareness we occupy; the remaining field of potential awareness is completely excluded from our narrow band of reality. At EvolveIndy, our therapists and counselors offer comprehensive and evidence-based drug and alcohol rehabilitation. If you or a loved one is suffering from addiction, visit us at EvolveIndy.com to learn more about how we can help!
Contracted States of Consciousness Can Be Useful In Accomplishing Tasks, But Damaging As a Permanent Brain State
This contraction of consciousness is a very useful state for accomplishing tasks that require extreme focus and attention to detail in the short term, but in the addicted individual, it becomes a pathological state of narrow fixation, repetition, and eventually ritualistic behavior. The brain adapts to this state of hyper-focus and the subsequent positive feedback from the reduction in anxiety (fear) that the drug provides. We essentially train our brain to work against its own innate programming to expand.
Consciousness in Contracted Brain States

There is a central tenant in modern neuroscience that conveys the basic idea of how thoughts become behaviors hard-wired in the brain; this is the idea of “neurons that fire together, wire together”.5 When groups of neurons repeatedly fire together they form what is called a neural network. Neural networks are thought to represent hard-wired “circuits” of our conscious experience, behavior, and memories in our brain’s architecture. Their activation creates a signature pattern of brain activity. Additionally, there are patterns of brain activity that are always occurring, whether we are in our waking state or in states of altered consciousness (such as deep sleep, dreaming, etc.). These patterns of ongoing activity are thought to represent a neural correlate of consciousness (NCC) and are postulated to be the framework that builds our conscious experience.6 These patterns of activity are modified from sensory inputs to improve our understanding of the world around us and can be built from a nearly infinite number of neuronal connections, representing a nearly infinite number of brain states or slices of consciousness. In a contracted brain state, the number of possible patterns of activity is reduced to a much smaller subset. These certain patterns of activity become reinforced by the coordinated firing of neurons driven by a narrow focal point of external stimuli. If the reward (reduction of fear being a highly-prized reward in our brain) of obtaining or ingesting that stimulus is large enough, the brain adapts to these patterns of activity and essentially begins to recode itself with access to a much more limited number of activities states.
Epileptic Seizures As an Example of Contracted Brain States
The most grievous example of a contracted brain state is what happens during an epileptic seizure; instead of an alteration of the synchronous and differentiated firing of high informational complexity, the patterns of brain activity become rigidly synchronous and simple. Consciousness becomes altered and narrowed to a very limited band of functioning in the person having an epileptic seizure. Patterns of brain activity are selected from a very simple, limited number of possible brain states and repeated until the seizure state is arrested.
The Process of Drug Addiction Follows a Similar Pathology to Epileptic Seizures
The process of drug addiction and the subsequent contracting of consciousness follows a similar pathology as the epileptic seizure: rigidity in brain activity, narrowing of the selection of possible brain activity states, simplification and reduction of neural entropy, and the reinforcement and adaptation to a small subset of brain activity patterns. The brain ceases to function in its innate, immense processing and integrative abilities, given the focus on an external object, and the sole purpose of its function becomes the maintenance of a contracted slice of awareness. Treatments for drug addiction that reinforce rigidity in brain activity (black-and-white thinking) and induce fear and anxiety (a punitive consequence of relapse, either through the criminal justice system or from social isolation from self-help groups) should all be regarded as highly dubious, based on this conceptualization of addiction as a form of contracted consciousness/brain states. The therapy intended to treat addiction may well reinforce its hold on us more deeply in these models of treatment.
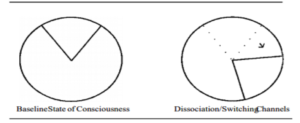
Dissociation Changes Consciousness and Brain States But Doesn’t Expand Them
One of the common issues in early drug addiction recovery is a phenomenon known as pseudo-transcendence. The idea here is that we shift our narrow band of focus within the 360° potential of awareness to another restricted area within the circle. If we were to imagine our drug addiction experience as watching the same television program over and over, we simply switch the channel to a new program and repeat the cycle of repetitively viewing a new program. Instead of expanding the repertoire of brain states and patterns of brain activation, we are simply replacing a small set of highly predictable activations with a different small set of highly predictable activations. Switching addictions from drugs to sex, gambling, working, people-pleasing, and all manners of dissociative behavior are not uncommon in early recovery processes. The addicted brain has been well trained to work in narrowing bands of focus to achieve the resolution of painful internal trauma and adapts easily to these familiar patterns with a new, novel external stimulus. And again, the more these patterns of brain activity occur together, the more deeply they’re ingrained in our behavior and breadth of conscious awareness.

Channel-Switching Therapies: Effective Reprieve or New Addiction Unto Itself?

Channel-switching therapies can be effective as a reprieve from the previous behavioral patterns, leading to a reduction in anxiety and the compulsive behaviors utilized to self-medicate. They can also quickly become a new source of fixated and compulsive behavior, as the idea here isn’t the resolution of painful internal states, but the management of anxiety caused by these states through the change in attention and focus. The psychoactive, mood-altering medications (SSRIs like Prozac, gabapentin, mood stabilizers like Abilify, and anxiolytics like Klonopin), often dispensed to addicts in early recovery, are a prime example of channel-switching, as they alter consciousness without any expansion of consciousness. Some reduce brain activation or interfere with new neuron development, and provide quick (or moderately quick) management of distressing symptoms; none of these medications help the addict confront the underlying issues driving their contracted state of awareness, and potentially separate them further from discovery due to their dissociative effect.
The Problem with Opioid MAT (Medication Assisted Treatment) Therapy
Long-term opiate maintenance therapy is the epitome of dissociative therapies. Dr. Stuart Gitlow, past president of the American Society of Addiction Medicine, says, “The drug that we’re replacing is a dangerous one that will kill you, and we’re replacing it with a drug that allows you to go back to work and have money in your pocket and allow you to live normally again”.7 In Wisconsin’s 2016 Calendar Year Report on Opioid Treatment Programs, however, 6669 of 9568 patients in opioid treatment programs (69%) were funded by Medicaid, which implies that the majority of the population receiving these treatments are either unemployed, under-employed, or disabled, given that this is a key qualifier for these benefits.8 So yes, substitution MATs may be preventing or reducing overdose deaths, but probably fulfilling the genuine return to productivity as Dr. Gitlow claims. Additional issues with MATs, and why they should be viewed as a dissociative therapy at best, are the further impairment of neuronal circuit plasticity, continued integration of maladaptive brain states that develop from opiate misuse, and, in general, keeping the addicted person subservient to a process of ritualistic drug use as a rewarding behavior. At Evolve Indy, we specialize in using short-term buprenorphine (only for a few days) to aid in opioid detox. To learn more about our treatment facility, our detox unit, and our rehabilitation programs, visit us at EvolveIndy.com.
A Note About Mindfulness and Other “New Age” Psychotherapies
Transcendental meditative practices and certain “new age” psychotherapeutic techniques also fall into this realm of channel-switching consciousness, as they function to distract attention from the internal source of the problem through fixation on a repeated mantra or affirmation. 12-step programs can also dip into the realm of a channel-switching therapy, as when priority is given to the social interaction the group provides, or relief of internal anxiety through mere attendance replaces the actual application of the spiritual principles divulged in 12-step literature as a program of recovery. As should be clear, pseudo-transcendence or channel-switching is clearly a shift in consciousness from one plane of maladaptation to another.
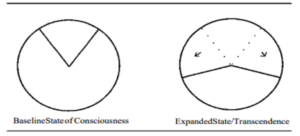
Expanded Consciousness is a Path to Recovery

The brain is amazing in its ability to metamorphize; it is possible and statistically probable that you can change your mind. With nearly an infinite number of possible brain activation patterns available each moment to become temporally and spatially linked, the odds are highly in our favor to change our utilization of Metzner’s metaphorical “sphere of awareness”. In this expanded field of consciousness, we occupy 60°, 180° or 360° of the sphere of awareness. Here we may still be watching the repeated television program with some attention, but we also have awareness of the TV set itself, the room it occupies, all that is going on in the space around and inside you, the birds in the trees outside our windows, the clouds in the sky—we start to see the big picture and can further open our range of experience beyond a narrow slice of attention.
From This State of Expanded Consciousness, We Can Process Painful Trauma More Effectively
It is from this state of expanded consciousness that we can process the painful internal contents we have been avoiding with compulsive drug use and other addictive or channel-switching behaviors. Here we open the possibility of creating new associations in our brain structures and enforcing new and novel patterns of brain activity. Some techniques used for consciousness expansion, such as mindfulness meditation, can repair areas damaged by compulsive drug use and have shown efficacy in reducing drug cravings and anxiety, two key drivers of the addiction cycle.9,10 Carefully deployed transpersonal and body psychotherapy can help us to transcend our painful, traumatic experiences through purposeful acknowledgment, validation, and reintegration of the experiences. In body-oriented psychotherapy, a blending of sensorimotor and cognitive psychology is utilized to produce a cathartic release of both emotional and physical traumas; transpersonal psychology encourages the exploration of spiritual or transcendent aspects of the human experience.
To learn more about the advantages and disadvantages of mindfulness meditation, check out this evidence-based review of mindfulness here!
Exposing and De-identifying From Sources of Fear, Anxiety & Trauma
In both practices, the source of anxiety, fear, or trauma is exposed, leaned into, and gradually detached and disidentified from our psyche. From this place of transcendence, which is a temporary state of expanded consciousness, we can create transformations in our awareness of consciousness, brain states, emotions, perceptions, and worldview. It is also from this place of expanded awareness that the spiritual principles of 12-step programs could be more meaningfully applied and accessed for sustaining recovery and personal growth. Viewing transformation as an ongoing life process (as suggested by 12 literature) wherein many layers will be shed, many brain states will be configured, and traumas are encountered and purged is paramount to continued recovery in this model of awareness.
An Integrated Model of Addiction Treatment?

Our current models of addiction treatment have progressed from viewing addiction as a moral failing only treatable through punitive means and social abandonment, to a medical model based on the assertion of addiction as a symptom or manifestation of a diseased brain state that can be managed by medications, TSF programs, and, when needed, criminal justice interventions. While becoming an effective management tool that could be argued to eventually open a space where the real issues can be handled, it’s time to investigate a new model of addiction and its treatment. A proposed treatment model would incorporate some aspects of the current system, but also include treatments that facilitate: The resolution of internal pain and traumas, the expansion of consciousness, the facilitation of access to an increased array of brain states, and the transformation of self and socially destructive behaviors. A program that deals with these issues, in addition to reintegrating the drug user into productive society, all seems necessary to help them move from a place of compulsive fixation and narrow focus to a fulfilling recovery and eventually a transformed life.
To learn more about our brain chemistry in addiction and recovery, check out my blog on low dopamine and the underlying brain disease that causes addiction here!
Closing Thoughts: Pioneering A New Way Forward in Addiction Treatment
While we have made significant strides in the last century in humane care for many who are suffering from substance abuse, we are still far from providing transformational addiction care and recovery management. Ineffective forms of psychotherapy and programs that rely solely on TSF are the standard of care across most of America’s existing treatment landscape. Long-term replacement therapies and psychoactive drugs for “symptom” management seem to be providing the best clinical evidence of efficacy in our current model for managing most drug dependencies, however, there is a concern that this strategy is keeping people safe, but stuck in a dissociative or contracted state of consciousness and unable to realize the full benefits of recovery and transformation. A proposed update to the existing model is an integrative practice that incorporates the following strategies: complete and prolonged detoxification using advanced nutritional, phytotheraputic, and, when indicated, short-term MAT therapies to commence recovery; a combination of psychosomatic and transpersonal individual psychotherapeutic and group therapeutic activities; cardiovascular exercise; a diverse array of creative activities to stimulate new brain pattern activation; mindfulness meditation practices and other conscious expanding exercises that facilitate an experience of transcendence and a platform for transformation. In contrast to the current models that use TSF as the foundational structure, in the transformational model TSF would be deployed after a significant period of detoxification, physical recovery, and consciousness-expanding exercises were underway and a later phase of the program. The idea is to introduce the participant to the self-described “spiritual, not religious program” of the 12 steps in a condition where they can integrate the program’s principles into their transformational process. As important here is that the individual feels they have autonomy in the choice to utilize 12-step programs as a platform for continued growth and that principles resonate with their own expanding sphere of awareness. The aforementioned techniques are good starting points for developing a transformational addiction treatment approach, and advancing from the current model of addiction management. The combination of consciousness expansion techniques with some of the existing architecture within the current addiction management system could be a new frontier for addiction treatment and the expansion of consciousness of society as a whole.
If you or a loved one suffer from substance abuse and addiction, reach out to our clinical team for help at EvolveIndy.com.
Works Cited:
- Kownacki, R. & Shadish, W. Does Alcoholics Anonymous work? The results from a meta-analysis of controlled experiments. Subst Use Misuse. 34 (14), 1897-1916 (1999)
- Ferri, M., Amato, L., & Davoli, M. Alcoholic Anonymous and other 12 step programmes for dependence. https://doi.org/10.1002/14651858.CD005032.pub2
- Schwartz, R. et al. Opioid Agonist Treatments and Heroin Overdose Deaths in Baltimore, MD 1995-2009. AM J Public Health. 103 (5), 917-922 (2013)
- Metzner, R. Addiction and transcendence as altered states of consciousness. J Transp Psych. 26, 1-17 (1994)
- Lowell, S. & Singer W. Selection of intrinsic horizontal connections in the visual cortex by correlated neuronal activity. Science. 255, 209-212 (1992)
- Ward, L. The thalmic dynamic core theory of conscious experience. Consciousness and Cognition. 20, 464-486 (2011)
- https://www.statnews.com/2017/05/15/medication-assisted-treatment-what-we-know
- https://www.dhs.wisconsin.gov/publications/p02115-16.pdf
- Goyal, M et al. Meditation programs for psychological stress and well-being: a systematic review and meta-analysis. JAMA Intern Med. 174 (3), 357-368 (2014)
- Tang, Y., Tang, R., & Posner, M. Mindfulness meditation improves emotional regulation and reduces drug abuse. Drug and Alcohol Dependence. 163 (1), S13-S18 (2016)

